Medicare Part D, Prescription Drug Plans for Those Who Qualify
Out-Of-Pocket Expenses Explained
The prescription drug coverage is the one, which covers the gap between the original Medicare and prescription drugs. When you have the original Medicare, you will have basic drug cover and many benefits of the prescriptions. This is where part D comes in handy to give you supplements insurance. In order to get this, you need to have a private insurance cover, which will give you the cover. There are different requirements that one needs to have in order to benefit from this plan. You need to have Medicare part A and part B in order to get the cover. This means that you cannot have part D without part A and part B. You also need to know that you cannot access part D if you are accessing part C. Members will need to contribute monthly premium of part D to their part B premium or any over medical premium they owe. The part D is usually meant to cover upfront costs on premiums, with the savings on deductibles making these drugs quite affordable.
Details of This Cover
Part D cover has loads of different details, and some of the affordable cover details include:
- Discount offers of drugs if you bug through mail or pharmacy
- Cover when you take the general brand name of drugs
- More savings in generic drugs until the year 2020
- 50% discount when buying brand-name prescription drugs
Costs of Medicare Part D
You will need to pay a fixed monthly premium and your insurer will have the responsibility of taking the bigger share in covered costs of drugs. This coverage is ideal for people who have a stable income and can qualify to get the cover easily. However, you need to know there are different details in the cover of part D, which makes it much easier for one to choose cover based on types of drugs, benefits, premiums, and doctor networks.
Who Should Get Part D?
If you are a senior and your medical costs and not covered by the original Medicare, you and use this part to access the cover. This way you will always have access to drugs at a cheaper rate through the private insurer. However, you will need to have part A and part B in order to get all the benefits of this cover. Many people want to get this cover and will need to make sure they have a good private insurance company to give out better results.
What is the Part D Late Enrollment Penalty?
If you do not meet the eligibility requirements for Medicare Part D and you enroll in your Part D late you will be penalized. This penalty will be for all the months you did not have prescription coverage. The penalty might be waived if you had prescription drug coverage from an employer or union that was covering as much as Medicare Part D was going to cover. Otherwise, you will be charged the penalty fee for late enrollment. If you meet the eligibility requirements for Medicare Part D and enroll on time you will not have to worry about paying the penalty fee for the remainder of the time you will have Part D coverage. This is to say the fee is split up into affordable monthly payments.
What About the Enrollment Periods That Happen Each Year?
Each year you can make changes to your Part D plan. This will happen in two open enrollment periods. The first open enrollment period will be for switching from your Medicare Advantage plan back to Original Medicare. This is also the time of the year when you can make changes to your Part D plan. If you would like different prescription coverage than you had the year prior, now is the time to make these changes. Also, if you would like to disenroll in your Advantage Plan there will be a special enrollment period for this.
What are Special Enrollment Periods?
These are special enrollment periods throughout the year. Say if you move you can make changes to your Medicare Advantage Plan and your Part D coverage. If you meet the eligibility requirements for special enrollment, you will need to act fast. The window of opportunity to make changes does not stay open very long.
What are Some Circumstances That Might Create a Special Enrollment Period?
Some of the circumstances are if you move. This is not just if you move from one state to another. These circumstances could mean that you were recently released from jail or prison, or if you move to an institution that does not accept your current plan. Also, included in a special enrollment period is if you lose your current coverage. There could be many reasons for you to lose your current coverage. This could be that your employer or union changed the coverage and now you are not eligible for prescription coverage. If there were changes in your plan’s contract with Medicare you might be forced to choose another Part D plan. This is something that does not often happen, but when it does, it creates a special enrollment period for anyone on those plans.
When am I Eligible for Medicare Part D?
To (“Medicare Eligibility Requirements For 2018 and 2019”) meet the eligibility requirements for Medicare Part D, you must have Medicare Parts A and B. You must be paying the premiums on Parts A and B. You do not have to be enrolled in a Medicare Supplement Plan, or qualify for Part D coverage. You will need to keep paying your Part B premium even if you do enroll in a Supplement or Advantage plan.
What are the Part D Premiums?
Part D Prescription Drug Plans are provided by Medicare-approved private insurance companies. Each of these private insurance companies is permitted to charge whatever they want. It is difficult to explain what the total premium price you will pay is. The premiums will vary from carrier to carrier and from plan to plan. Your Part D Prescription Drug Plan premium is usually tied in with the Advantage Plan or Supplement Plan.
What is the Part D Prescription Drug Plan Deductible?
Like the premium plan for Part D, the deductible for Part D will vary. Medicare puts a cap on the deductible an Advantage Plan or Supplement Plan can charge. For 2018, this premium, deductible cap is $405. However, despite what you might think, there might be an easier way to go about getting your Part D coverage and not having to pay this deductible. There are Medicare Plans that will cover Part D with no deductible. What you pay, again will vary depending on the Advantage or Supplement Plan you choose.
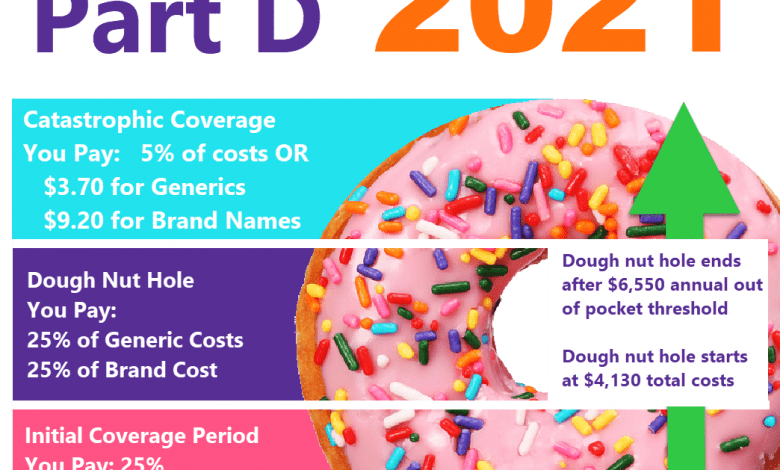
What Does Out-Of-Pocket Expense Mean?
Out-of-Pocket expenses are what you will pay. This is what you will pay when your Medicare or Advantage or Supplement plan does not cover. Whether you have original Medicare or an Advantage Plane you will have an out-of-pocket expense to pay. This is to say if you are having outpatient surgery and there is a co-insurance you will have to pay for this part of the surgery. The co-insurance is an expense that is uncovered (“P&C Insurance Property Section 1: Insurance Terms and Related Concepts”) (“What Is Medicare? – [PDF Document]”) by your Advantage Plan you will have to pay for it out-of-pocket.
What is the Maximum Out-of-Pocket I Will Have to Pay?
Again, the maximum out-of-pocket expense will vary depending on your plan. You will want to select your plan carefully based on what they do and do not cover. There are Advantage and Supplemental plans that cover expenses such as vision, hearing, and dental. If these are expenses that are important for you to have coverage on then you should choose a plan that covers these options. However, each plan has its own out-of-pocket maximum each year for each participant.
How do I Minimize My Out-of-Pocket Expenses?
This will depend on what types of conditions you have. If you have a chronic condition and need to see a doctor regularly, you might not want to pay a low premium for your Advantage plan and Part D plan. The higher the premium the lower the out-of-pocket expenses you will have to pay each year. So, if you pay a premium of $79, you will have to pay co-payments and co-insurance payments. However, these might not add up to the expenses you would face if you had high deductibles for your insurance premium. The higher the deductible, the lower the monthly premium. This could add up quickly, though.
What is the Difference Between Co-payment and Coinsurance?
A co-payment is something you will pay the doctor or specialist each time you go to the doctor. The co-payment is something that you cannot get around. This is the expense that you have to pay or your portion of the medical expense of the doctor’s visit. Coinsurance is an amount you will have to pay if you have surgery or some other procedure done. The coinsurance is something you will have a percentage of the total cost of the procedure. So, if you go in for surgery and the total cost is $1,000, and you have a coinsurance of 20%, your cost for the procedure would be $250. A co-payment is usually a specified dollar amount and coinsurance is usually a percentage.
